Dear Professor Loren Cordain,
One should only grab a pen or, in this case, a keyboard and write an open letter if they want to make a clear and meaningful point. Competence in the subject is an advantage. We hope we meet both criteria.
First of all, please let us express our appreciation for your work in the field of human nutrition science. We particularly appreciate your work as we have learned a lot from you. We are convinced that the changes your work has triggered will result in a considerable shift in nutrition science and help return to a reasonable and healthy diet which conforms to human evolution, or at least it will help with its scientific and exact description. As you suggest, there must be a single, optimal diet for all Homo sapiens: an authentic Paleolithic Diet.
We are writing this open letter because we want to respond to the recent criticism you expressed regarding Ketogenic Diets. We chose to publish an open letter, because thus we can inform laypeople about a professional debate which may be of public interest. You are a distinguished professional in the field of nutrition science and recently have expressed opinions on Ketogenic Diets, which have reached a wide range of people.
We would like to address some of the points you made, which, in our opinion, contain scientific mistakes. This is necessary as, on the one hand, we are the founders and operators of the medical center with the most experience of Paleolithic, Ketogenic, Carnivore and Paleo-Ketogenic (PKD), etc. diets; on the other, our institute has applied and perfected your theoretical work, and, as a result, has been successfully treating incurable diseases, e.g. type 1 diabetes and cancer. We do not primarily talk about theories, we talk about clinical practice. We are writing our letter in hope of informing those who might feel uncertain because of the mentioned mistakes, and we also would like to encourage you to revisit certain statements you have made. Both of these goals are important to us, but the most important is scientific truth. If, however, facts, figures and clinical practice prove you right, we are willing to reconsider our position.
We are aware that these lines may generate conflict, but we can assure you that our priority is the pursuit of scientific truth and not interest. Almost all our clinical activities are based on the theoretical research you and your colleagues had done, for which we are very grateful to you.
To be able to see clearly, we first need to consider some fundamental and important aspects.
In nearly 10 years of clinical practice, it has become evident to us that Paleolithic nutrition should constitute a diet of animal meat and fat supplemented by certain and a limited amount of plant-based foods. We note that, based on our clinical results, animal-based nutrition is a biological necessity for human nutrition, and plant-based nutrition is of culinary value only. Such a diet, in many cases, generates ketosis, which means that the ATP molecules the body needs are produced by means of oxidation of fatty acids and ketone bodies in the mitochondria. This is important because we can produce more ATP per one unit of fat in the mitochondria than of one unit of sugar in the cytoplasm. At this point, the question arises: why would evolutionary selection, which always moves towards a minimized and the most effective direction, put glycolysis at the forefront if it takes so much more energy? Besides, during the production of one unit of energy, more reactive oxygen radicals are formed than during the production of the same energy from fat. That is, the fat-based mode is not only more energy efficient, but also safer when it comes to the prevention of cell and tissue damage.
The other equally important but less understood aspect is that healthy Paleolithic nutrition does not cause increased intestinal permeability. The issue of intestinal permeability in relation to Paleolithic nutrition has just been, quite rightly, introduced to the wider public through your research. You produced a great summary about the interrelation between intestinal permeability and the development of autoimmune diseases. This was our starting point when we began to test the intestinal permeability phenomenon with our patients in 2015, first in collaboration with a London laboratory and then in our own laboratory. This is why we are grateful to you. Dutch researchers’ and our own test results have shown that intestinal permeability is not normalized by means of the popular Paleolithic nutrition or classic Ketogenic Diet. Since these two criteria (ketosis and normal intestinal permeability) were not met by Paleolithic Diet or classic Ketogenic Diet alone, the nutritional approach which meets both criteria had to be called differently for technical and didactic reasons in order to distinguish their clinical effectiveness. The concept (and term) of Paleolithic nutrition in the popular sense has led to confusion, which you have previously highlighted. At the moment, there is utter chaos in what the term “Paleolithic” actually means, what kind of nutrients belong to the Paleolithic Diet, and whether homeopathy, with its unestablished background, can be part of a Paleolithic Diet which is based on purely scientific principles. Consequently, in order to enable precise scientific interpretation, we had to give a different name to our diet. This is how the term “Paleolithic Ketogenic Diet” (PKD) was coined.
It is very important to understand, Professor, that our system is not the outcome of a selection of ready-made bits and pieces of certain positive dietary elements. We did not set up arbitrary rules and frameworks, our diet was designed as part of therapeutic processes and is based on clinical responses, symptomatology, and laboratory and the imaging diagnostics. We were able to evaluate the feedback accurately because we have nearly 20 years of experience in internal medicine and at emergency units of hospitals, which preceded diet-based healing, and which made it possible to analyze the results correctly. In Hungary, for instance, fragments of the Paleolithic Diet were introduced by a layman who had no physiological experience and qualifications, and as a result your work became widely known in a distorted way. Distinction from this necessitated the use of different terminology. Of course, this was a local feature of Hungary, yet, later it turned out that similar distortions occurred at an international level, too. So, retrospectively, we think we made a good decision when we started to use the term “PKD,” and when we did not define it as one of the Paleolithic Diets, otherwise it would have got confused with the popular Paleolithic Diet. This is an existing phenomenon today and, unfortunately, some people, incorrectly in our opinion, talk about Paleolithic Diets.
A pillar of the concept of your Paleolithic Diet is that only one diet is healthy and optimal for the human race. We are also of the same view, as this is obviously the result of known biological laws. While there are a good number of Ketogenic and Paleolithic Diets on the “health market,” from a scientific and physiological point of view, there is only one which constitutes healthy eating.
There are many diets that can help with achieving ketosis (Ketogenic Diets), but only one of these does not cause intestinal permeability. This diet is also perfectly suited to the criteria of the Paleolithic Diet. Today, there is no plant-based food in our diet which could have been there in the Paleolithic Age.
We consider the abovementioned explanation to be an extremely important aspect because, according to our experience, researchers of Ketogenic and Paleolithic nutrition do not understand the use of this distinctive terminology.
As you have many followers and there are deeply flawed and contradictory opinions circulating on the Internet, in order to come clean regarding views of the Palaeolithic Diet and to present a scientifically correct interpretation of ketosis, it is our duty to set things right.
Without this rather long introduction, non-professional audiences may not be able to fully understand our reaction, which is why clarification of the concepts was necessary. Therefore, unpleasant this may be, we would like to call your attention to our scientific findings: the thousands of patients and tens of thousands of patient data and substantial clinical experience. We believe that thorough consideration of the evidence provided will convince you to reconsider your views about ketosis and Ketogenic Diets. In our opinion, the clinical introduction of the Paleolithic Diet cannot be achieved without a thorough understanding of the essence of ketosis.
By definition, any diet that promotes ketosis may be called a Ketogenic Diet. However, ketosis and Ketogenic Diets are not synonymous. Indeed, Ketogenic Diets can have side effects, but they are not caused by ketosis; rather, they are caused by ingredients which make a diet non-Paleolithic and are found in a given Ketogenic Diet, including vegetable oils, dairy products, and other foods. To avoid further misunderstandings, it is useful to call such a diet a classic Ketogenic Diet. The difference between classic Ketogenic and Paleo-Ketogenic Diets, with particular regards to side effects and applicability in cancerous diseases, is described in more detail in an earlier article we published (Tóth et al., 2017).
As for the specifics, we have the following comments on your criticism:
“By default, Ketogenic Diets are mainly composed of animal fats and proteins along with very small quantities of carbohydrates (< 50 g or < 200 kcal) from plant foods.”
We are convinced that in order to be able to refute an argument, the argument must be fully understood.Your claim that Ketogenic Diets usually contain animal fat and meat is incorrect; in fact, the exact opposite is true. Generally, Ketogenic Diets are based on vegetable oils and dairy products, as we can see it at the epilepsy departments of medical clinics, in the literature on Ketogenic Diets, or in the recommendations of so called “charismatic bloggers.” As mentioned above, for the sake of clarity, we term this diet as classic Ketogenic Diet. Don’t be misled by the fact that close versions of this diet are also known in the literature as, e.g., the modified Atkins Diet, Insulin-Lowering Diet, Low-Glycemic Index Treatment (LGIT), or the very low-calorie Ketogenic Diet (VLCKD) you also mentioned. The latter name is problematic, since the calorie content does not reveal much about the healthy or non-healthy properties of a diet. Eskimos, for instance, observe a healthy diet, which contains only meat and animal fat, although their calorie intake is high. The diets listed above do not really differ in their components. They are all variations of the same diet based on vegetable fats and dairy products and additional, clearly not Paleolithic, foods. The official recommendations for Ketogenic Diets explicitly exclude foods containing red meat and cholesterol. Let’s be frank, there are very few mainstream medical professionals who can integrate the Paleolithic aspect, so they promote a defective Ketogenic Diet lacking this Paleolithic aspect. Of course, charismatic bloggers have their own responsibility, but in this case they simply seem to copy these bad recommendations without criticism.
To sum up, there is only one Ketogenic Diet based on animal fats, plant fats, dairy products and excluding other non-Paleolithic ingredients completely; this is the Paleo-Ketogenic Diet described and applied by our team. Although we could mention the Carnivore Diet, which is based on foods of animal origin, but the Carnivore Diet is not Ketogenic and, thus, does not deliver the benefits associated with ketosis. The Atkins Diet you criticize is a non-Ketogenic Diet too. The reason for this is that a drastic reduction in carbohydrate intake is not enough for ketosis for which a proper fat to protein ratio is required. If a diet is truly Ketogenic, that is, the right fat to protein ratio is established, there is no need to worry about the “protein ceiling” phenomenon and its consequences.
Returning to your highlighted sentence, we cannot tell whether you were talking about PKD or Ketogenic Diets in general. In the references, you mention many studies about the Ketogenic Diet, which, actually, examined the classic Ketogenic Diet, but you do not cite our scientific reports on the Paleo-Ketogenic Diet. We do not assume that this is intentional, nonetheless it is a serious professional mistake.
”Unless VLCKD diets include dairy products (milk, yogurt, cheese) in their daily menus…”
Here, you suggest that Ketogenic Diets do not contain dairy products. This is not true. The most common ingredient in Ketogenic Diet recipes is whipped cream. Based on what we know about the negative effects of dairy products, we cannot believe that they would be able to counteract the negative effects of any diet. The only Ketogenic Diet that does not contain milk and dairy products is the Paleo-Ketogenic Diet.
Fruits
Your claim may give the impression that vegetables and fruits may save us from the damaging effects of meat and fat. This suggestion coincides with the recommendations of official medical bodies, with mainstream literature, and with the recommendations of “mainstream alternative therapists.” Studies which focus on the benefits of fruits are mostly based on epidemiological research. Epidemiology is inadequate to establish cause-and-effect relationships and to control the effects of real world phenomena. Only intervention can be used to determine cause and effect and for us, clinicians dealing with patients, nutrition intervention is a daily practice. Clinical experience has shown that regular consumption of fruits, alongside either western or Paleolithic Diets, has a number of negative effects. These negative changes show in laboratory parameters: fruit consumption increases, for instance, LDL cholesterol, uric acid, triglyceride, TSH, blood sugar, and insulin levels, even to the abnormal range. We experience that it stops weight loss or promotes weight gain, increases water consumption and water retention, can cause swelling of the feet, high blood pressure, can cause abnormal sweating, and, in many cases, it degrades sleep quality. Tiredness, sleepiness, difficulty in concentration and even abdominal cramps may occur as a result. According to research, fructose can increase the risk of certain tumors, such as pancreatic tumors. Scientific research has also shown that fructose greatly reduces the conversion of inactive vitamin D to active vitamin D by blocking 1-alpha hydroxylase; even a minimal increase in plasma fructose level may cause the latter. The negative effects of vegetables are very similar to those of fruits. Of course, not only fructose has a negative effect, but also other ingredients of fruits and vegetables. What do fruits and vegetables contain which are not contained in meat and fat? Are they essential parts of our diet? We need to answer these simple questions if we want to define the place of vegetables and fruits in essential human nutrition. Based on our experience and results, neither vegetables nor fruits are essential parts of human nutrition, they do not contain ingredients we need, and which meat and fat do not provide.
The applicability of nutrient requirement tables
The biggest flaw in research based on nutrient requirement tables and official RDIs is that they were developed on the basis of research and tests in Western nutrition, and on the other hand, they do not take into account the nutrient interactions within the body. Interaction with carbohydrates is the most important aspect of the bioavailability of minerals and vitamins. This is a little known and researched but very important aspect, and the earliest biochemistry textbooks also present this relationship as a fact. Therefore, RDI values are not relevant for any low carb diet. You would like to put the Ketogenic Diet in line with Western nutrition recommendations, while you basically questioned the Western diet by laying the foundations of the Palaeolithic Diet. This is an irreconcilable contradiction.
The numbers in the official bodies’ recommendations can only be valid for the unhealthy Western diet, but they are certainly invalid besides ketosis and, especially, PKD. Thus, these recommendations cannot be used to challenge the idea of ketosis. According to the nutrient requirement tables, software, and recommendations the official daily carbohydrate requirement is 130 g; however, from a physiological point of view, human carbohydrate intake is zero if adequate amounts of fat and protein are included in our diet (Westman, 2002). Again, zero is not just a value calculated on the basis of a theory. Many of our patients eat up to 50-70 g of protein (200-280 g of meat) and 150-200 g of animal fat and nothing else on a daily basis for many years.
We would like to add that the classic Ketogenic Diets can actually cause nutrient deficiencies, but specific evidence for this is not to be found in the nutrient requirement tables and in the deviations from the recommended intake. Nutrient requirement tables and calculators do not say anything about complex nutrient interactions in the human body. The question of whether or not a particular diet actually causes nutrient deficiency is most likely to be determined by identifying the blood level of the particular nutrient or by identifying the clinical deficiency symptom of the particular nutrient.
”Nevertheless, as I will emphasize later on, contemporary Paleo Diets also accomplish these same health goals but without the detrimental long-term nutritional and metabolic effects elicited by Ketogenic Diets.”
You are suggesting that Paleolithic Diets can achieve the same results as Ketogenic Diets, but there are no side effects in Paleolithic Diets. This statement is relative and may be true in case of weight loss, lowering of blood sugar and insulin, or lowering high blood pressure (the latter only if the Paleo Diet does not contain too much fruit), which can be achieved with both Paleolithic and Ketogenic Diets. Unfortunately, this claim is not true in case of inflammation control, autoimmune diseases, tumors or normalization of increased intestinal permeability. Although Paleolithic and Ketogenic Diets bring us one step closer to healthy eating, both have ample side effects.
Paleolithic Diets, if not low carb, may result in obesity and high blood sugar. The risk of cardiovascular disease and cancer is significantly increased by fruits and vegetable oils (both appearing in the popular Paleolithic Diet). We have had many patients who had been suffering from cancer and autoimmune diseases for several years while observing the popular Paleolithic Diet. We can support this by relevant data.
Acid-base balance
The part of your criticism regarding acid-base balance is based on misleading ideas of ketosis circulating on the Internet, rather than on physiological facts. Unfortunately, the concepts of ketosis and ketoacidosis are frequently confused, largely due to the misinterpretation and of standard diabetology and nephrology as well as hoaxes. We can confirm that ketosis is not identical with ketoacidosis and ketosis does not cause ketoacidosis either. One hundred years ago, ketoacidosis was treated with low-carb diet. I would also like to highlight that we have not yet met clinical cases of ketoacidosis or acidosis during PKD; if your statement were true, we should have seen relevant cases. Given our extensive therapeutic experience, the chances of such cases left unnoticed are practically zero.
You claim that vegetables and fruits protect us from acidification. There is no physiological basis for this statement. Let us start with the physiological facts of the acid-base balance.
1. All forms of nutrition contribute to net acid production. That is, your claim that the consumption of plants and / or carbohydrates is different from the consumption of meat and fats in terms of the direction in which the acid-base balance shifts is untrue. The amount of carbon dioxide produced in the cells is important when it comes to the question of acid-base balance; it depends largely on the amount of food you eat. As in the PKD diet, and any other diet causing ketosis, patients take in smaller amounts of food than in the popular Paleo or Western Diet, thus Ketogenic Diets are less demanding for our buffer systems. This is a very simple mathematical interrelation: the compensation reserve is much bigger during ketosis. We should mention that starvation also causes net acid production as the breakdown processes of the own reserves persist.
2. The breakdown of each protein / amino acid would move the acid-base balance of the plasma into an acidic range, in case of both animal or vegetable protein. Veterinarians are well aware, for example, that the feeding of otherwise grazing animals with cereals, due to the extreme amount of plant protein load, can cause metabolic acidosis and even the death of the animal. Without meat and fat! In humans, for example, high acidic shifts are caused by the following plant nutrients: cereals, plums, nuts, peanuts, legumes, almonds, biscuits, pastas. This category also includes fruits, vegetables and dairy products. High carbohydrate intake also increases the production of acetic acid and lactic acid. Animal and vegetable fats are mostly in the neutral category.
3. Carbohydrate consumption, especially when associated with anaerobic physical exercise (glycolysis), increases the level of intracellular and plasma lactate, thus also pushing the plasma pH into the acidic range. In case of high carbohydrate intake, the accumulation of bacteria’s metabolic products would also push the blood into the acidic end of the pH scale, as bacteria produce L-lactic acid as well as D-modifications, which the liver is unable to convert into pyruvic acid, but its acidic character prevails. This is a constant burden on the body’s alkaline reserves, which can be seen from the decrease in the urine base excess of urine. There are many top athletes who did not win competitions as a result of this process.
4. The pH depends greatly on metabolic intensity, which is clinically the most testable in TSH levels. In ketosis, the metabolic intensity is 2-3 times lower than in case of carbohydrate-based nutrition.
5. When ATP is produced from fatty acids and ketone bodies in the mitochondria (rather than from glucose in the plasma), it significantly reduces the number of hydrogen ions in the plasma and in the intracellular space by operating a nanomotor containing ATP synthetase, and, therefore, it can be considered to be a powerful buffer system.
But the point here is: whatever we eat, the human body works wonderfully thanks to evolution and, in most cases, it is, ultimately, capable of permanent biological adjustments owing to its multiple buffer systems. There are at least five buffer systems in the body that constantly ensure that the body’s pH is always within the same narrow range, regardless our diet. This can be overwritten by severe forms of diseases, but not due to ketosis. In the alternative health world of the Internet, it has become a habit to assign symptoms like those of reflux, bloating, and all kinds of specified or unspecified symptoms, to acidosis. In fact, a healthy person never develops acidosis when observing a Ketogenic Diet.
The only condition in which a healthy person can develop acidosis is sudden carbohydrate intake following starvation. Such cases were documented at the end of World War II, when the concentration camps were liberated and cities were recaptured, and the starving people suddenly got large amounts of carbohydrates, which in many cases caused their death. However, in these cases, carbohydrates and the depletion of alkaline reserves were to be blamed and not fat and protein.
Strangely enough, diabetology recurrently returns to the issue of alleged acidosis caused by low-carbohydrate diets. Our response to one of the related case studies, which contains additional information, can be read here (Tóth, 2015).
Potassium
Again, with regards to potassium, the question arises whether or not it is possible to draw scientific conclusions from the recommendations of Western diet which you refuted. Please note that clinical experience confirms that potassium is the parameter in the blood that is minimally altered even by the most severe diseases and even in case of Western nutrition. Unfortunately, the case of potassium has been significantly overreacted by representatives of internet-based alternative medicine, which resulted in many unscientific conclusions; as a consequence, people started to take potassium supplements, which may have serious side effects. As far as PKD is concerned, we have at least ten thousand potassium tests in our possession, and I can safely say that the potassium level is always in the normal range during PKD. In very rare cases, when potassium levels are low due to underlying diseases, the problem is resolved with PKD in a short time.
Sodium
We do not understand what brought you to the overall conclusion that the salt intake of Ketogenic Diets is high. The ketogenic property alone does not reveal anything about how much salt the diet contains. In this respect, I think we should not refer to a fictitious table. However, salt intake is closely related to the amount of glucose and fructose intake as intestinal epithelial cells take glucose from the intestinal lumen to the apical surface through the so-called sodium-dependent glucose transporter. The intestinal epithelial cell can only use sodium, in order to transport sugars, from the intestinal lumen, i.e. sodium is needed for glucose transport. This also means that the more carbohydrates one consumes, the more sodium one needs. The process is self-regulating and the excess sodium passes through the kidneys without causing diseases. The followers of popular Paleolithic Diets often report on this phenomenon, and they feel food to be very salty, which was not the case before.
Calcium
“Unless VLCKD diets include dairy products (milk, yogurt, cheese) in their daily menus, it is difficult or impossible to meet the RDI (1000 mg) for calcium, simply because animal and plant fats which represent the bulk of energy (65-75%) in VLCKD contain virtually no calcium”
This RDI requirement does not have to be met. This is a repetition of the previous error based on a fundamentally incorrect definition. The majority of indigenous peoples have a fraction of 1000 mg of Ca intake per day, while they do not consume dairy products either. Eskimos only consume meat and fat, yet they show no symptoms of calcium deficiency (e.g. symptoms suggesting osteoporosis) until they swap their diets for Western nutrition. In contrast, astronauts’ plasma calcium levels and calcium levels in their bones are drastically reduced within days of space travel, despite consuming dairy products. Thus, professionals of NASA or Roscosmos even try to recover as much calcium as possible from the urine of astronauts. The example of the Eskimos you put forward reflects the fact that bone density alone reveals little about bone health. It is well known, for example, that the Japanese have low bone density, still incidents of bone fractures are rare, which is mainly due to the fact that they traditionally do not drink milk and do not eat dairy products. The calcium stored in grazing animals’ meat and in our own bones is perfectly enough to maintain health. The expectation of satisfying RDI is physiologically unfounded in either ketosis and in other cases. In fact, osteoporosis, as the example of astronauts shows, does not have much to do with the amount of calcium intake. The processes behind osteoporosis are governed by other biochemical laws: osteoporosis is caused by nutrients that absorb calcium from the bones (thus enabling the functioning of one of the abovementioned acid-base buffer systems). Such dietary elements are dairy products. The consumption of milk and dairy products also increases the risk of osteoporosis and fractures (despite the fact that they contain a lot of calcium). Bone density, as in the case of astronauts, is mainly controlled by the intensity of muscle power on the bones, which is around zero in weightlessness. Similarly, if we fall ill and are bound to bed for 2-3 weeks, we lose bone density. We would like to draw your attention to a figure which displays one of our patients’ bone density. Well-designed ketosis does not cause osteoporosis; on the contrary, it cures it without drugs or supplements (Figure 1).
It should be noted here that, contrary to your statement, neither the classic Ketogenic Diet nor the PKD causes muscle loss; to the contrary, they help to maintain muscle mass. Muscle loss can only happen if one does not take in carbohydrates or fat and consumes little protein. Thus, amino acids of own muscles are used for energy production.
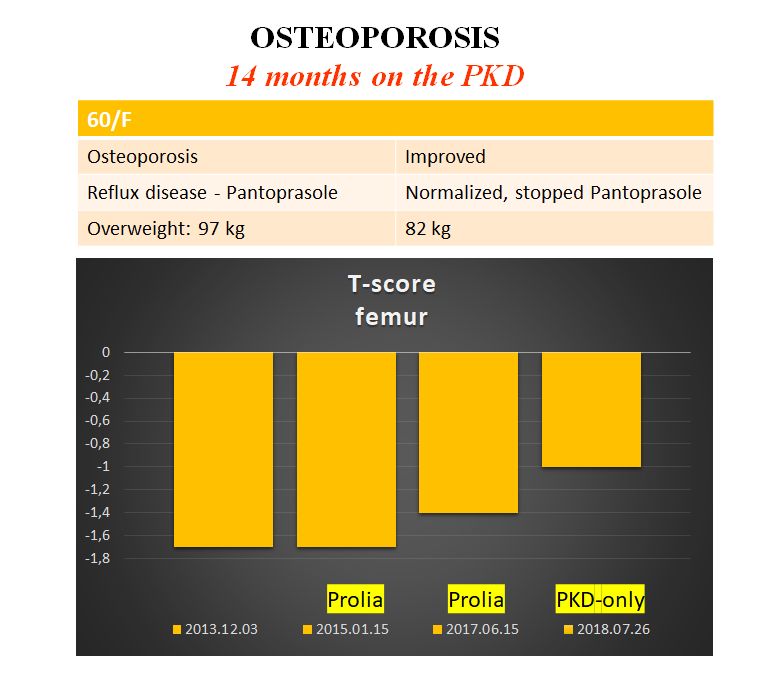
Figure 1
T-score of a patient with osteoporosis previously. After discontinuing the drug called Prolia, the bone density increased on PKD alone. Source: Clemens and Tóth 2018.
Magnesium
Magnesium deficiency brings up the issue of the RDI again, which presents an arbitrary and debatable number in case of magnesium. Magnesium balance simply cannot be interpreted without nutrition as a whole. At this point, we think you have not read our study published in the Journal of Evolution and Health, in which our team presented the magnesium levels of 50 patients on PKD and ketosis (Clemens et al., 2017). 49 out of the 50 patients had normal levels of magnesium. For the sake of comparison, magnesium levels may be low in up to 40-75% of the same patient populations on Western diet. In this article we explain how it is possible that a low magnesium diet can provide normal magnesium levels, while a Western diet that contains much more magnesium does not provide adequate magnesium levels in most cases.
Vitamin C
We are embarrassed because we need to refer to our own study on vitamin C again, which, apparently, slipped your attention (Clemens and Tóth, 2016). Vitamin C is another good example of how the role of nutrients cannot be interpreted without the food environment as a whole. Vitamin C is not a quantitative issue, as is the case with many other vitamins and microelements. Taking vitamin C tablets and eating a lot of fruits or vegetables alone will not protect us from cancer, cardiovascular diseases, or an early death. That is, quantitative compliance with RDI alone will not solve anything. The peoples living above the Arctic Circle do not consume any plants for most of the year, yet they do not show symptoms of vitamin C deficiency. Moreover, their health indicators are far better than those on Western diets. The key to solving the vitamin C problem, that is, the Inuit Paradox, is the glucose ascorbate antagonism (GAA), which means that, because of their molecular similarity, glucose and vitamin C are competing at many points in the body’s functioning, and they are competitive antagonists in getting into the cells. This also means that it is not only the amount of vitamin C we consume that matters, but also the food environment. In addition to carbohydrates, oxalate and flavonoids in vegetables and fruits also inhibit vitamin C absorption. Vegetables and fruits are therefore not a good source of vitamin C, even though they contain a lot of it.
Folate
As you noted, one of the best sources of folate is liver; it is also a source for vitamin C, vitamin D and many other vitamins. Whether people like or dislike liver mostly depends on cultural and habitual factors. All of the indigenous peoples of the world appreciate liver, and it is found among the traditional recipes of all nations. If modern humans, who moved away from both their Palaeolithic and national (traditional) eating habits, are reluctant to consume liver and offal in general, it the result of a partial phenomenon of evolutionary mismatch you often mention. Scientific truth is independent from this. The framework of this paper does not allow deep explanation, but the evolutionary solution is the only good solution. That is, we have to eat liver and offal as they cannot be replaced by any other man-made pill and supplement.
Ketogenic Diet: Is it so bad that you can only take risks and use it in advanced cancer patients?
We would also like to respond to the argument that a risky diet which may be risky for a healthy person can still be beneficial for someone with an advanced disease. This argument often arises during the criticism of the Ketogenic Diet. In fact, there is no bad diet that would be useful in any disease and a healthy diet does not only have a positive effect on diseases. PKD is not a healing diet. PKD is effective in cancer, epilepsy and other diseases because PKD is a healthy diet. This is because all the people on Earth, including the healthy and the sick, have the same optimal diet: PKD or animal meat-fat based diet, as Walter Voegtlin called it in his masterpiece titled Stone Age Diet. Returning to this healthy diet is equally good for the sick and the healthy, as the sick person, on the one hand, needs it more, and on the other hand, they are less tolerant of deviations from it.
A defence of Ketogenic Diets
Certain methodological features, which are not obvious to people outside of the clinical practice, should also be mentioned in defence of Ketogenic Diets. The side effects of a classic Ketogenic Diet, although obvious, are not at all clear as to how they relate to the side effects associated with Western diets. Obviously, the question has not been raised before because mainstream medicine denies that the Western-type diet would have side effects. Instead, it looks for causes in genetics and environmental impacts. In fact, we do not have a correct starting point for comparing the side effects of the classic Ketogenic Diet and the Western diet. The reason for this, on the one hand, is that Ketogenic dietary studies tend not to involve non-Ketogenic control groups and, on the other, they do not control the effects of the drugs. Most of the Ketogenic Diet studies are related to epilepsy. For example, for those outside the field of epilepsy studies, it is not known that epilepsy drugs distort metabolism and increase the loss of certain ions and nutrients to such a great extent which certainly cannot be attributed to the Ketogenic Diet. However, mainstream medicine, due to its self-protective reflexes, tends to link side effects with non-mainstream diets, rather than questioning the safety of drugs.
Clinical experience vs. published studies
You may ask how we can make confident assertions on grounds of the small number of case studies we published. There are technical reasons for this. You, who started the Paleolithic movement decades before others, have to realize that it has not been integrated into mainstream medicine and medical recommendations, thus perhaps you can understand the obstacles we encounter when publishing our results. It should be noted here that in 2017, the Polish Pediatric Society included the Paleo-Ketogenic Diet in its therapeutic protocol for inflammatory bowel disease. Although it is a positive sign, it is still a strong exception. The processing of large amounts of data is not easy in a hostile environment and without any financial support, as thorough scientific work is time and energy consuming and we proceed with it slowly due to the large number of patients we treat on a day-to-day basis. This is why, often, in the eyes of colleagues socialized in conventional medicine, our references to clinical experience is unacceptable. By the way, clinical experience was a guiding principle for the development of medicine until hundreds of years ago, before the increased influence of the pharmaceutical industry.
As a sign of our respect, we hereby offer you to look at our data about any disease or test result at any time. We do this in the hope of settling this scientific controversy and take back supervision of the Paleolithic Diet from self-appointed influencers. We, physicians and researchers, work to make the Paleolithic Diet a mainstream medical method so that it means the same in Washington, Vladivostok, Melbourne, and Budapest. We would also like to prove what you said: there is an ideal and genetically determined diet for all people. This is the scientifically proved Paleolithic Diet, which excludes vegetable oils, flour, and supplements. If we do this, doctors will have the opportunity to cure and prevent many civilizational health problems.
Yours sincerely,
Csaba Tóth and Zsófia Clemens
References
Clemens, Zsófia, Tóth, Csaba (2016) "Vitamin C and Disease: Insights from the Evolutionary Perspective," Journal of Evolution and Health. Vol. 1: Iss. 1, Article 13.
Clemens, Zsófia, Csaba Tóth. “Paleolithic Ketogenic Diet (PKD) in chronic diseases: clinical and research data.” Invited presentation at the 6th Symposium of the German evolutionary medicine and health. https://evolution-medizin-gesundheit.org/wp/wp-content/uploads/2018/04/Programm_2018_V1.pdf
Clemens, Zsófia, Dabóczi, Andrea, Tóth, Csaba (2018) "The Paleolithic Ketogenic Diet may ensure adequate serum magnesium levels," Journal of Evolution and Health. Vol. 2: Iss. 2, Article 6.
Tóth C. (2015) Comment on ”Ketoacidosis associated with low-carbohydrate diet in a non-diabetic lactating woman: a case report"
https://www.researchgate.net/publication/305710427_Comment_on_Ketoacidosis_associated_with_low-carbohydrate_diet_in_a_non-diabetic_lactating_woman_a_case_report
Tóth C, Dabóczi A, Chanrai M, Clemens Z. (2017) Comment on “Systematic Review: Isocaloric Ketogenic Dietary Regimes for Cancer Patients” by Erickson et al. Journal of Cancer Research and Treatment. Vol. 5, No. 3, 2017, pp. 86–88.
Westman, Eric C. “Is dietary carbohydrate essential for human nutrition?,” The American Journal of Clinical Nutrition, Volume 75, Issue 5, 1 May 2002, pp. 951–953.
The open letter was originally published in Immunoreica
2019-11-20
 Rehabilitáció csak online elérhető
Rehabilitáció csak online elérhető
 E-mail: paleomedicina@gmail.com
E-mail: paleomedicina@gmail.com


